Human Saliva May Prove Key to Fighting Drug-Resistant Bacteria
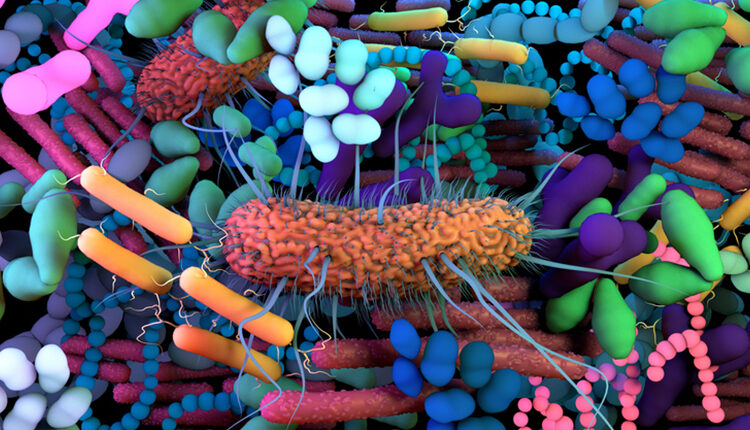
Drug-resistant pathogens are a growing problem. But according to one study, we may not have to look further than our own spit for a cure.

According to the United States Centers for Disease Control and Prevention, more than 2.8 million antibiotic-resistant infections occur in the US annually, resulting in more than 35,000 deaths. The agency’s 2019 report reflects various levels of threat posed by 18 antimicrobial-resistant bacteria and fungi, with three more on a watch list.1
Infections caused by such pathogens can result in everything from drug-resistant respiratory infections to necrotizing fasciitis.1 This is especially concerning in immunocompromised populations.2 But it’s a growing problem overall, and the need to develop new kinds of antibiotics is urgent.
PEPTIDES TO THE RESCUE
A new study conducted at the University of Minnesota is suggesting that antimicrobial peptides inspired by a salivary protein may prove to be an alternative to traditional antibiotics. Researchers from the School of Dentistry developed GL13K, an antimicrobial peptide derived from the structure of the human salivary protein, BPIFA2. To assess its potential impact on drug-resistant bacteria, they teamed up with investigators from the Department of Experimental and Clinical Pharmacology.
The recently published research focused on whether the peptide could kill common drug-resistant bacteria and bacterial biofilms, and whether the bacteria would become resistant to it. To determine this, they tested LGL13K and DGL13K, two amino acid components of the new peptide against Gram-negative, drug-resistant bacteria.2,3
PROMISING RESULTS
The researchers discovered that both versions of the peptide killed common Gram-negative bacteria. Although the bacteria did develop a resistance to the LGL13K peptide, it did not in the case of the DGL13K peptide, nor did it inhibit the DGL13K’s ability to kill these bacteria.
The researchers concluded that peptides developed from salivary protein can be effective in combating bacteria, including drug-resistant, gram-negative bacteria. One of the study’s authors, Elizabeth Hirsch, PharmD, FCCP, noted, “We were able to show significant in vitro activity against multidrug-resistant bacteria tested in this project. There are very few antibiotics on the market with activity against these organisms, specifically, resistant Pseudomonas aeruginosa, Klebsiella pneumoniae, and Acinetobacter baumannii. Exploring this peptide further in clinical development will be important for potential future treatment options.”2
The researchers plan to continue tracking the bacteria to determine if and when they eventually do become drug resistant. The research helps lay the groundwork for additional investigation and identifies DGL13K as a promising antimicrobial peptide candidate for further development. And not a moment too soon.
REFERENCES
- United States Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019.
- University of Minnesota Twin Cities. Treating Antibiotic-Resistant Infections With Peptides Inspired by Human Saliva.
- Gorr SU, Brigman HV, Anderson JC, Hirsch EB. The antimicrobial peptide DGL13K is active against drug-resistant gram-negative bacteria and sub-inhibitory concentrations stimulate bacterial growth without causing resistance. PLoS ONE. 2022;17:e0273504.

