Tips for the Nonsurgical Treatment of Periodontitis
The main goals of nonsurgical periodontal therapy (NSPT) are to remove and control supra- and subgingival microbial biofilms, eliminate and control inflammation, and eliminate and control systemic and local risk factors that contribute to disease development and progression.
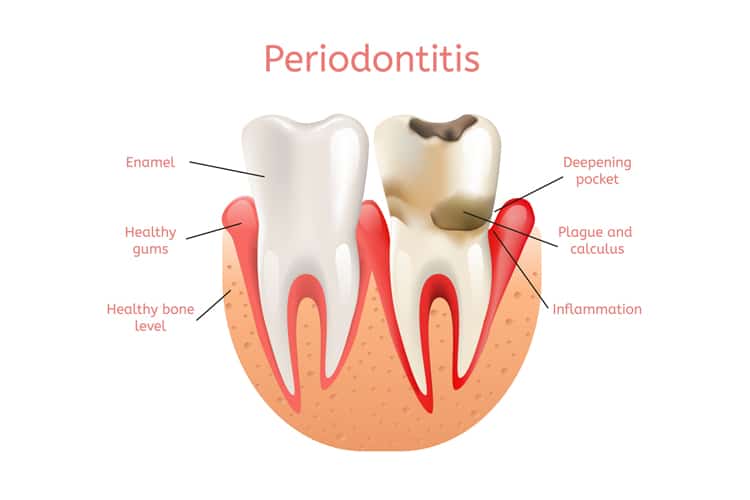
The main goals of nonsurgical periodontal therapy (NSPT) are to remove and control supra- and subgingival microbial biofilms, eliminate and control inflammation, and eliminate and control systemic and local risk factors that contribute to disease development and progression. Depending on the degree of bony involvement, effective NSPT may minimize or eliminate the need for surgical intervention.
Photo Credit: Tera Vector / iStock / Getty Images Plus

Controlling Systemic Risk Factors
Several risk factors have well established associations with both periodontal and systemic diseases, such as diabetes, smoking, stress, immunodeficiency, medications, obesity, hormones, and nutrition. For optimal treatment results, systemic risk factors must be modified or eliminated.
Photo Credit: boonchai wedmakawand / iStock / Getty Images Plus

Eliminating Local Risk Factors
A variety of tooth-related local risk factors can predispose a patient to developing an inflammatory periodontal lesion. These can be grouped into three general categories: anatomical, tooth position, and iatrogenic. While local risk factors are not considered to be a direct cause of periodontitis, they contribute to biofilm development, increased biofilm pathogenicity, and calculus retention. Local risk factors can be modified and/or eliminated—and, in fact, periodontal therapy should not be considered complete until all local risk factors have been addressed.
Photo Credit: danielzgombic / iStock / Getty Images Plus

Behavior Modification
Effective plaque control is a requirement in nonsurgical and surgical periodontal therapy. Assessment, motivation, and reinforcement of oral hygiene should be performed at each appointment. Recent research evaluating the association between oral hygiene and periodontitis showed that the risk of periodontitis increased by twofold to fivefold in patients with poor oral hygiene.
Photo Credit: PIKSEL / iStock / Getty Images Plus

Scaling and Root Planing
Meticulous scaling and root planing is the most critical component of initial periodontal therapy. The primary goals of scaling and root planing are to significantly reduce or eliminate subgingival microbial loads, remove subgingival calculus, remove soft and diseased cementum, and smooth roughened root surfaces.
Photo Credit: alex-mit / iStock / Getty Images Plus
Antimicrobials
The adjunctive use of systemic antibiotics with scaling and root planing is known to yield a statistical difference, but arguably not a clinically significant difference. Studies that have evaluated the use of locally delivered antimicrobials—such as chlorhexidine chips, doxycycline hyclate gel, and minocycline spheres—report modest clinical benefits. Whether the benefit is clinically significant depends chiefly on expert opinion and not statistical evidence.
Photo Credit: busracavus / iStock / Getty Images Plus
Reevaluation
Clinicians are advised that reevaluation is not the end-point of active periodontal therapy—it is part of a decision matrix. Periodontal status should be thoroughly reassessed at 4 weeks to 6 weeks following the nonsurgical phase of treatment, as the greater part of healing is completed by 6 weeks, but collagen maturation might continue for up to 9 months.
Photo Credit: enot-poloskun / iStock / Getty Images Plus

Periodontal Maintenance
Achieving long-term periodontal stability requires an effective periodontal maintenance program and patient compliance. Maintenance generally includes a reevaluation to determine the patient’s periodontal status, evaluation of systemic and local risk factors, supragingival scaling and polishing, scaling and root planing of residual probing depths—particularly those that exhibit bleeding on probing.

