
Smarter Full-Arch Implant Planning
Artificial intelligence and advanced digital workflows are transforming full-arch implant planning by improving accuracy, efficiency, and collaboration
As digital dentistry continues to evolve, artificial intelligence (AI)-powered planning is becoming a cornerstone of predictable, prosthetically driven full-arch implant rehabilitation. Upon successful data importation into implant planning software and accurate registration, digital tools facilitate a prosthetically driven implant planning approach. This enables a comprehensive visualization of the ideal prosthetic tooth positioning, restorative space, osseous architecture, and soft tissue contours, ensuring a precise and predictable treatment outcome. AI is gaining significant attention in dentistry, particularly in digital implant planning.1
AI-based multimodal image registration for cone-beam computed tomography (CBCT) and intraoral scanning (IOS) has demonstrated high accuracy, time efficiency, and consistency, making it a valuable tool for presurgical implant planning.2 Additionally, AI-driven segmentation of the mandibular canal in CBCT enhances efficiency and reliability in implant planning.3 However, manual verification remains essential to mitigate potential errors and ensure precise anatomical interpretation.
Systematic reviews and meta-analyses note that the use of fewer than five implants per arch to support a fixed prosthesis in completely edentulous maxillae or mandibles achieves survival rates comparable to those obtained with five or more implants per arch. The analysis demonstrated no statistically significant difference (p < 0.05, 95% confidence interval) between these approaches.4
Intentionally tilted implants demonstrate comparable clinical performance to axially positioned implants, providing significant advantages such as reduced need for bone grafting and minimized prosthetic cantilevers. These benefits are achieved without compromising implant survival rates or contributing to increased marginal bone loss, making tilted implants a predictable and effective treatment option in implant-supported prosthetic rehabilitation especially maxilla.5 However, implants should be placed in an axial orientation whenever feasible, as tilted implants increase the complexity of both surgical and prosthetic procedures.
With implant-assisted complete-arch removable dental prostheses (IACRDPs), the angulation of implants relative to each other plays a critical role in ensuring optimal prosthetic function, stability, and load distribution. This contrasts with implant-supported complete-arch fixed dental prostheses (ISCFDPs), in which the primary concern is often the angulation of the abutments rather than the implants themselves. However, in certain cases, individual abutments, such as locator abutments, allow for a specific range of acceptable divergence between implants, accommodating minor misalignments while maintaining prosthetic retention and function. Nevertheless, greater divergence among implants increases the likelihood of prosthetic complications, potentially compromising retention, stability, and long-term success. Therefore, precise evaluation and planning of implant angulation are essential to minimize prosthetic challenges and enhance the predictability of implant-supported and implant-assisted prosthetic rehabilitation.7
 One of the key advantages of a digital workflow, particularly in digital implant planning for full-arch implant restorations, is the optimized selection of abutments, especially multi-unit abutments, which are frequently required for this type of rehabilitation. The decision-making process for abutment selection plays a crucial role in determining implant positioning and angulation. In particular, the selection of the height of multi-unit abutments is critical for maintaining long-term marginal bone stability and may also influence soft tissue stability.
One of the key advantages of a digital workflow, particularly in digital implant planning for full-arch implant restorations, is the optimized selection of abutments, especially multi-unit abutments, which are frequently required for this type of rehabilitation. The decision-making process for abutment selection plays a crucial role in determining implant positioning and angulation. In particular, the selection of the height of multi-unit abutments is critical for maintaining long-term marginal bone stability and may also influence soft tissue stability.
Several studies have reported that shorter abutments (≤ 1.5 mm) are associated with greater marginal bone loss compared to taller abutments, highlighting the importance of precise abutment selection in digital implant planning.7-12 Abutment height should be at least 2 mm to minimize marginal bone loss.12 The required restorative space, encompassing both vertical and horizontal dimensions, is a critical consideration in prosthetic rehabilitation, as it directly influences the selection of prosthetic materials and the design of the final prosthesis. The minimum vertical restorative space, measured from the crestal soft tissue to the antagonist occlusal plane, varies depending on the type of prosthesis:13,14
- FP-1 prosthesis: 7 to 12 mm
- FP-2 and FP-3 prostheses: ≧ 12 mm
- RP-4 prosthesis: ≧ 15 mm
- RP-5 prosthesis: 8 to 9 mm
Beyond vertical space, the horizontal restorative space must also be evaluated to ensure adequate prosthetic support, esthetics, and biomechanical stability. A comprehensive three-dimensional assessment of restorative space is essential for achieving long-term functional and esthetic success in ISCFDPs and IACRDPs.
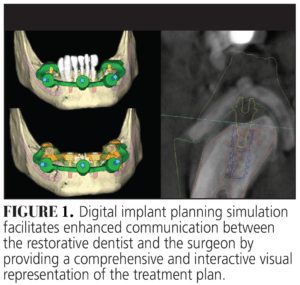
One of the significant advantages of digital implant planning is that it enables surgeons and restorative dentists to collaborate effectively by discussing and confirming implant positions, as well as simulating the surgical procedure prior to actual implant placement (Figure 1). Additionally, this technology facilitates patient involvement in the treatment planning process. By allowing for precise preoperative communication, digital implant planning minimizes the risk of misunderstandings or misinterpretations, ultimately enhancing treatment accuracy and predictability. With continued advancements in AI and digital workflows, clinicians can expect even greater precision, efficiency, and confidence in full-arch implant treatment planning.
References
- Alfaraj A, Nagai T, AlQallaf H, Lin WS. Race to the moon or the bottom? applications, performance, and ethical considerations of artificial intelligence in prosthodontics and implant dentistry. Dentistry Journal. 2025;13(1):13.
- Elgarba BM, Fontenele RC, Ali S, et al. Validation of a novel AI-based automated multimodal image registration of CBCT and intraoral scan aiding presurgical implant planning. Clin Oral Implants Res. 2024;35(:1506-1517.
- Ntovas P, Marchand L, Finkelman M, Revilla-León M, Att W. Accuracy of artificial intelligence-based segmentation of the mandibular canal in CBCT. Clin Oral Implants Res. 2024;35:1163-1171.
- Daudt Polido W, Aghaloo T, Emmett TW, Taylor TD, Morton D. Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29:154-183.
- Lin WS, Eckert SE. Clinical performance of intentionally tilted implants versus axially positioned implants: a systematic review. Clin Oral Implants Res. 2018;29:78-105.
- Rabbani S, Juszczyk AS, Clark RK, Radford DR. Investigation of retentive force reduction and wear of the locator attachment system with different implant angulations. Int J Oral Maxillofac Implants. 2015;30:556-563.
- Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T. Effectiveness of implant therapy analyzed in a swedish population: prevalence of peri-implantitis. J Dent Res.2016;95:43-49.
- Galindo-Moreno P, León-Cano A, Monje A, Ortega-Oller I, O’Valle F, Catena A. Abutment height influences the effect of platform switching on peri-implant marginal bone loss.Clin Oral Implants Res. 2016;27:167-173.
- Nóvoa L, Batalla P, Caneiro L, Pico A, Liñares A, Blanco J. Influence of abutment height on maintenance of peri-implant crestal bone at bone-level implants: a 3-year follow-up study. Int J Periodontics Restorative Dent.2017;37:721-727.
- Pico A, Martín-Lancharro P, Caneiro L, Nóvoa L, Batalla P, Blanco J. Influence of abutment height and implant depth position on interproximal peri-implant bone in sites with thin mucosa: A 1-year randomized clinical trial.Clin Oral Implants Res. 2019;30:595-602.
- Blanco J, Pico A, Caneiro L, Nóvoa L, Batalla P, Martín-Lancharro P. Effect of abutment height on interproximal implant bone level in the early healing: A randomized clinical trial. Clin Oral Implants Res. 2018;29:108-117.
- Chen Z, Lin CY, Li J, Wang HL, Yu H. Influence of abutment height on peri-implant marginal bone loss: A systematic review and meta-analysis. J Prosthet Dent. 2019l;122:14-21.
- Sadowsky SJ, Fitzpatrick B, Curtis DA. Evidence-based criteria for differential treatment planning of implant restorations for the maxillary edentulous patient. J 2015;24:433-446.
- Sadowsky SJ, Hansen PW. Evidence-based criteria for differential treatment planning of implant restorations for the mandibular edentulous patient. J Prosthodont. 2014;23:104-111.
This originally appeared in Nagai T, AlQallaf H. Precision planning in full-arch implant rehabilitation. Decisions in Dentistry. 2025;11(4):32-35.

