Digitally Driven Dual-Arch Transformation Restores Function and Confidence
When a 55-year-old patient requested fixed implant solutions with no removable options, a fully digital workflow delivered a seamless transformation from surgery to smile. Using advanced imaging, guided surgery, and zirconia restorations, clinicians achieved exceptional esthetics, durability, and patient satisfaction.
 A 55-year-old woman with advanced periodontal disease and generalized tooth mobility sought a fixed implant solution to restore her smile and function. Leveraging a completely digital workflow, from digital smile design and cone-beam computed tomography (CBCT) planning to guided surgery and immediate provisionalization, her care team executed a dual-arch, full-arch rehabilitation that combined precision, efficiency, and esthetic excellence. This case highlights how digital dentistry and modern materials are redefining full-arch implant treatment outcomes and patient experiences.
A 55-year-old woman with advanced periodontal disease and generalized tooth mobility sought a fixed implant solution to restore her smile and function. Leveraging a completely digital workflow, from digital smile design and cone-beam computed tomography (CBCT) planning to guided surgery and immediate provisionalization, her care team executed a dual-arch, full-arch rehabilitation that combined precision, efficiency, and esthetic excellence. This case highlights how digital dentistry and modern materials are redefining full-arch implant treatment outcomes and patient experiences.
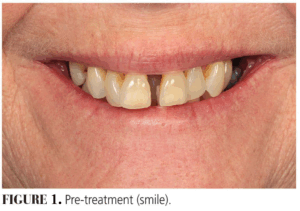
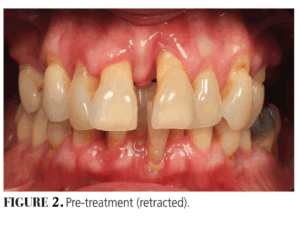 A 55-year-old woman presented with the desire for a fixed implant option (Figures 1 and 2). No significant medical history was noted. A clinical exam revealed advanced periodontal disease with generalized Grade III mobility. An asymptomatic periapical lesion was present on #30. Supra-eruption of the mandibular anterior teeth was noted. Her existing vertical dimension of occlusion was acceptable. She had a moderate smile line.
A 55-year-old woman presented with the desire for a fixed implant option (Figures 1 and 2). No significant medical history was noted. A clinical exam revealed advanced periodontal disease with generalized Grade III mobility. An asymptomatic periapical lesion was present on #30. Supra-eruption of the mandibular anterior teeth was noted. Her existing vertical dimension of occlusion was acceptable. She had a moderate smile line.
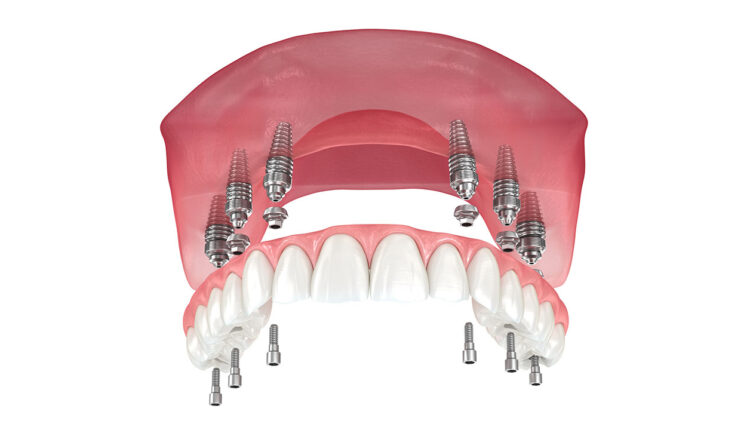
Treatment options of crown and bridge on implants and full-arch implant prostheses were discussed. The patient accepted proceeding with dual-arch full-arch implant prostheses. Utilizing a fully digital workflow, photographs were made and sent for digital smile design (Figure 3). Once the design was approved, a stereolithography file of the digital smile design was merged with an intraoral scan and CBCT imaging to plan for implant surgery. Six maxillary implants and four mandibular implants were placed by an oral and maxillofacial surgeon.
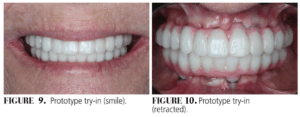
 Immediately following the surgery, appropriate multiunit abutments were placed and scan gauges were scanned. These scans were merged with the digital smile design to fabricate immediate provisional hybrid prostheses. Provisionals were printed using a ceramic-hybrid resin and placed the next day following immediate load protocol (Figures 4 and 5). After implant healing for 3 months, provisionals were removed, and scan gauges were placed and scanned to proceed with fabrication of prototypes and zirconia full-arch implant prostheses (Figure 6). Scans were verified chairside (Figure 7). Design changes were made to the provisionals (Figure 8) and prototypes were fabricated for try-in (Figures 9 and 10).
Immediately following the surgery, appropriate multiunit abutments were placed and scan gauges were scanned. These scans were merged with the digital smile design to fabricate immediate provisional hybrid prostheses. Provisionals were printed using a ceramic-hybrid resin and placed the next day following immediate load protocol (Figures 4 and 5). After implant healing for 3 months, provisionals were removed, and scan gauges were placed and scanned to proceed with fabrication of prototypes and zirconia full-arch implant prostheses (Figure 6). Scans were verified chairside (Figure 7). Design changes were made to the provisionals (Figure 8) and prototypes were fabricated for try-in (Figures 9 and 10).
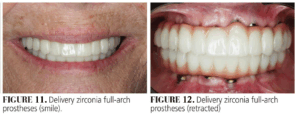
 After prototype approval, new scans of the prototypes were made and screw-retained maxillary and mandibular titanium bar with zirconia overlays were fabricated and inserted (Figures 11 and 12). Oral hygiene was reinforced and maintenance protocols established. An occlusal device was fabricated. The patient reported very high satisfaction with the treatment rendered.
After prototype approval, new scans of the prototypes were made and screw-retained maxillary and mandibular titanium bar with zirconia overlays were fabricated and inserted (Figures 11 and 12). Oral hygiene was reinforced and maintenance protocols established. An occlusal device was fabricated. The patient reported very high satisfaction with the treatment rendered.
 Full-arch rehabilitation has evolved dramatically from osseointegration discovery to today’s digitally driven workflows. Deciding between preserving natural teeth or proceeding with implant rehabilitation requires comprehensive assessment of dental history, medical factors, financial constraints, and patient expectations. Despite impressive long-term survival rates of 90% to 98% over 10 to 15 years, clinicians must remain vigilant about potential complications including peri-implant disease and technical failures.
Full-arch rehabilitation has evolved dramatically from osseointegration discovery to today’s digitally driven workflows. Deciding between preserving natural teeth or proceeding with implant rehabilitation requires comprehensive assessment of dental history, medical factors, financial constraints, and patient expectations. Despite impressive long-term survival rates of 90% to 98% over 10 to 15 years, clinicians must remain vigilant about potential complications including peri-implant disease and technical failures.
 Advanced materials, such as zirconia, have significantly improved durability and esthetics, while digital technologies have revolutionized treatment planning and execution through CBCT imaging, intraoral scanning, and guided surgery protocols. The integration of prosthetically driven planning, immediate loading, and refined surgical techniques continues to elevate the standard of care in full-arch rehabilitation. Treatment decisions remain highly individualized, requiring careful consideration of functional outcomes, esthetic goals, and patient preferences. Ongoing innovation promises even greater precision and predictability, ultimately enhancing our ability to restore not just oral function, but also confidence and quality of life for patients.
Advanced materials, such as zirconia, have significantly improved durability and esthetics, while digital technologies have revolutionized treatment planning and execution through CBCT imaging, intraoral scanning, and guided surgery protocols. The integration of prosthetically driven planning, immediate loading, and refined surgical techniques continues to elevate the standard of care in full-arch rehabilitation. Treatment decisions remain highly individualized, requiring careful consideration of functional outcomes, esthetic goals, and patient preferences. Ongoing innovation promises even greater precision and predictability, ultimately enhancing our ability to restore not just oral function, but also confidence and quality of life for patients.
This originally appeared in Chang B. The evolution of full-arch implant rehabilitation. Decisions in Dentistry. 2025;11(3):10-15.

