Bringing Oral Health to the Frontlines of Cancer Care
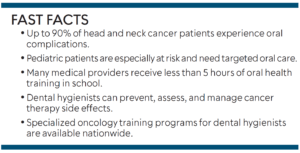
Despite the high rate of oral complications during cancer treatment, many patients receive little to no oral health guidance, highlighting the urgent need for dental hygienists to join oncology teams.
According to Global Burden of Disease data, cancer accounts for approximately 10 million deaths annually, representing roughly one in six global deaths.1 As the incidence of cancer increases, so too are the cancer therapeutics that directly impact the oral cavity.2 Dental complications can arise while a patient is undergoing cancer treatment, resulting in long-lasting effects years after treatment is complete.
Adverse side effects to cancer treatment include oral mucositis, xerostomia, osteonecrosis, acute periodontal disease, Candida infections, herpes simplex viral infections, and trismus. Approximately 40% of patients develop some form of oral mucositis.3 This percentage rises to 60% to 85% for patients undergoing hematopoietic stem cell transplantation and to almost 90% for patients treated with radiation plus chemotherapy for head and neck cancer.3 Oral complications can significantly affect patients’ quality of life, increase their financial burden, and delay cancer treatment. However, far too often, other medical concerns overshadow the oral assessment and management.2
Lack of Knowledge Among Medical Providers
Despite a high incidence of oral complications, most oncology patients are not educated on the importance of oral health throughout the course of their cancer treatment. Promoting oral health during cancer treatment is critical to improve patients’ quality of life. This requires increased awareness, prevention, and treatment by multidisciplinary care teams, including dental hygienists.2 Traditionally, nurses are the frontline providers in patient management. Unfortunately, nurses and other medical professionals do not receive much education on oral health.
The oral cavity is a recognized source of inflammation, yet approximately 70% of medical school curricula only include 5 hours or less of oral health content and 10% do not have any education or training in oral health.4 In a systematic review on nurses’ knowledge, attitudes, and practices regarding oral healthcare in cancer patients, studies found that nurses significantly vary in their understanding of oral diagnosis, treatment, and hygiene protocols.5 While some nurses may be aware of the potential oral complications, many lack the knowledge and/or confidence to assess and treat oral complications. Several studies indicated that nurses struggled to identify and treat xerostomia, dysphagia, and trismus. Deficiencies in the referral process and care coordination between healthcare and oral health professionals were also highlighted, emphasizing the need of standardized protocols, comprehensive assessments, and early intervention strategies.5
Children undergoing cancer treatment represent an especially vulnerable group, yet the surveyed nurses demonstrated less than adequate knowledge about providing oral care for pediatric patients receiving cancer therapy or hematopoietic stem cell transplantation.5 Highlighting this research is not to place blame but rather to emphasize the need for dental hygienists to become valued members of the oncology team.
Dental hygienists are well-positioned to serve as oral health advocates and educators. Dental hygienists should be working alongside nursing staff, alleviating their workload and responsibilities, to provide patient-centered care.
Although dental providers are experts in oral health, secondary complications associated with cancer treatment are complex. This new role can be challenging for dental hygienists initially, as they work in a nontraditional setting in a multidisciplinary team to treat medically complex patients. To aid in this transition, there are a few programs that offer continuing education specifically for oncology.
![]() Multidisciplinary Management of Head and Neck Cancers
Multidisciplinary Management of Head and Neck Cancers
The National Comprehensive Cancer Network’s Multidisciplinary Management of Head and Neck Cancers is an accredited program designed to meet the educational needs of physicians/oncologists, nurse practitioners, nurses, physician assistants, pharmacists, and other healthcare professionals who manage patients with cancer.6 This program offers 6 hours of continuing education, provides strategies for nutrition management, and reviews the importance of oral and dental evaluations for patients with head and neck cancers.
Integrative Oncology Patient Navigator Program
Maryland University of Integrative Health offers the Integrative Oncology Patient Navigator Program.7 Enrolled students have 2 years to complete 45 hours of continuing education. This program emphasizes the importance of holistic, complementary care in cancer and students will learn how to develop appropriate integrative care plans along with a patient’s healthcare team. A significant portion of this program focuses on the ability to evaluate current evidence-based complementary health approaches and how to educate cancer patients on choosing integrative therapies to enhance their cancer care journey.
National Network of Healthcare Hygienists’ Oncology Certificate
The National Network of Healthcare Hygienists (NNHH) created an oncology certificate for dental hygienists to learn about the specific needs of cancer patients and how to integrate a dental hygienist into an oncology setting.8 Upon completion of NNHH’s self-paced oncology program, students will be prepared to advocate for oncology patients’ oral health needs as well as prevent and treat oral side effects with evidence-based research, products, and technology. The curriculum covers the biology of cancer, oral side effects during cancer therapy, and residual oral side effects patients may experience into survivorship.
This program includes a pediatric section created by Katharine Martinez, MPH, RDH, an oral health educator at Phoenix Children’s Hospital and a pioneer in integrating dental hygienists into oncology care teams. In her modules, Martinez shares how her role was developed along with pediatric-specific oncological care models, treatment modalities, pharmacological considerations, and team-based applications. This program offers 18 hours of continuing education and a certificate of completion after passing a final assessment and completing a capstone project. The capstone project serves as a springboard to approach a local oncology treatment center to apply the knowledge and skills students learn during the program to create a position on a multidisciplinary care team.
Oral Health Integration
Oral health integration is part of each hospital’s strategic plan, but often healthcare systems are unsure as to how to implement this new model of care. A common thread all three of these programs share is the confidence dental hygienists gain to educate multidisciplinary oncology teams on the importance of establishing an oral health assessment, referral processes, and prevention and treatment protocols.
Conclusion
Dental hygienists have much to offer patients undergoing cancer treatment. It takes a team to treat cancer patients and the trajectory of healthcare is rapidly changing. As dental hygienists, it is up to us as a profession to advocate for these nontraditional roles and, ultimately, advocate for our patients.
References
- GBD Collaborators. Global, regional, and national age-sex specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-1788.
- Harris JA, Ottaviani G, Treister NS, Hanna G. An overview of clinical oncology and impact on oral health. Front Oral Health. 2022;3:1-8.
- Elad S, Yarom N, Zadid Y, Kuten-Shorrer M, Sonis S. The broadening scope of oral mucositis and oral ulcerative mucosal toxicities of anticancer therapies. CA Cancer J Clin. 2021;72:57-77.
- Haber J, Hartnett E, Allen K, et al. The impact of oral-systemic health on advancing interprofessional education outcomes. J Dent Educ. 2017;81:140-148.
- Sajwani AI, AlShdaifat M, Hashi F., Abdelghany E, Alananzeh I. The intersection of oncology and oral health: exploring nurses’ insights and practices—a systematic review. Support Care Cancer. 2024;32:137-152.
- National Comprehensive Cancer Network. Available at https://education.nccn.org/node/95906#group-tabs-node-course-default1. Accessed August 8, 2025.
- Maryland University of Integrative Health. Available at https://ce.muih.edu/browse/ce/courses/integrative-oncology-patient-navigatortraining#:~:text=This%20comprehensive%20professional%20training%20program,%C2%B7. Accessed August 5, 2025.
- National Network of Healthcare Hygienists. Available at healthcarehygienists.org. Accessed August 8, 2025.
From Dimensions of Dental Hygiene. September/October 2025; 23(5):9-10.