
Perio Update: The Danger of Residual Cement
The popularity of implant therapy has grown exponentially, and it is now the go-to treatment for tooth loss.
SUBSCRIBE TO THE PERIO UPDATE NEWSLETTER HERE
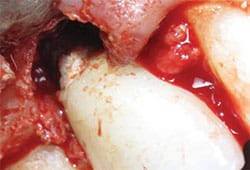
The popularity of implant therapy has grown exponentially, and it is now the go-to treatment for tooth loss. However, maintaining implants is not as easy as it may seem. This case study demonstrates the importance of ensuring that all residual cement has been removed (Figure 1), which often requires the use of a dental endoscope, in order to ensure implant health. The following case study demonstrates how residual cement was detected, the effects of leaving cement behind on an implant surface, and an appropriate course of treatment to support the long-term health of the implant.
Case Study

The patient is a healthy, nonsmoking 52-year-old woman with an unimpressive medical history. Tooth #19 had been extracted due to a failing root canal. A dental implant was placed 3 months post-extraction and the patient returned to her restorative dentist to place the implant crown. Five years later, she was referred for evaluation of implant #19, with bleeding and exudate noted on probing. Implant #19 showed no obvious signs of inflammation on initial visual inspection. However, palpating the buccal and lingual aspects yielded exudate. The circumferential probing depths measured 6 mm to 9 mm and there was less than 1 mm of buccal keratinized epithelium. The radiographic exam revealed bone loss to the second implant thread on the distal and the third on the mesial (Figure 2). There was no radiographic evidence of cement.
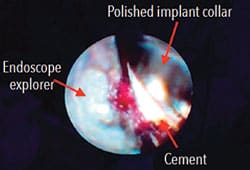
Under local anesthetic, the dental endoscope fiber was placed under the gingival margin and the crown margin and polished implant collar were inspected. Upon inspection, residual cement was noted on the buccal and lingual aspects (Figure 3). An ultrasonic scaler was used to remove the residual cement while simultaneously visualizing the area through the endoscope. This allowed for debridement without needless instrumentation, protecting the implant surface. The implant was carefully debrided until cement was no longer visible through the endoscope.

In addition to endoscopic treatment, the surface of the implant was decontaminated using glycine powder, followed by a 5-minute irrigation with 10% iodine solution.1 Finally, a Nd:Yag laser was used to perform a bacterial reduction of the pocket, with caution to prevent soft-tissue curettage.2 The patient returned for maintenance at 3-month intervals during which the implant surface was treated with glycine, iodine, and laser bacterial reduction at each visit.3 After 3 months, there were no signs of inflammation, exudate, or bleeding while palpating the buccal or lingual aspect or while probing. After 1 year, the pocket depths had reduced to 4 mm to 5 mm and radiographic exam shows some possible bone remineralization (Figure 4).
If this implant had been inspected with an endoscope at the time of restoration, more complete removal of residual cement would have been accomplished, reducing the risk of peri-implantitis. Considering these findings, clinicians must understand how to instrument around a dental implant to reduce the possibility of soft tissue contamination. Oral health professionals also need to consider that traditional periodontal flap procedures may still be necessary to treat peri-implantitis even after nonsurgical treatment with an endoscope.
References
- Slots J. Selection of antimicrobial agents in periodontal therapy. J Periodont Res. 2002;37:389–398.
- Abduijabbar T, Javed F, Kellesarian SV, Vohra F, Romanos GE. Effect of Nd:YAG laser-assisted non-surgical mechanical debridement on clinical and radiographic peri-implant inflammatory parameters in patients with peri-implant disease. J Photochem Photobiol B. 2017;168:16–19.
- Stein J, Hammacher C, Michael S. Combination of ultrasonic decontamination, soft tissue curettage and submucosal air polishing with povidone-iodine application for non-surgical therapy of peri-implantitis: 12 months clinical outcomes. J Periodontol. December 5, 2017. Epub ahead of print.
This case study originally appeared in Fortune N, Obrotka MA. Subgingival endoscopic visualization and treating peri-implantitis. Dimensions of Dental Hygiene. 2019;17(8):14–17.

