Classifying Periodontal Diseases
In 1989, a classification system was proposed that included five types of periodontitis: adult periodontitis, early onset periodontitis, periodontitis associated with systemic disease, necrotizing ulcerative periodontitis, and refractory periodontitis.

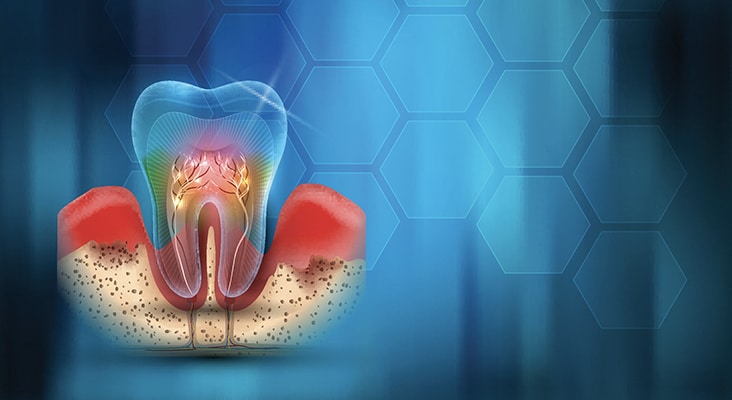
In 1989, a classification system was proposed that included five types of periodontitis: adult periodontitis, early onset periodontitis, periodontitis associated with systemic disease, necrotizing ulcerative periodontitis, and refractory periodontitis. This system was widely used among practitioners although a gingival disease component was missing and there was an overlap of disease categories. In addition, some criteria appeared to be unclear or inadequate. Given that changes were needed, in 1999, the classification system for periodontal diseases and conditions was updated. That system was based on an infection and host response concept. The 1999 system recognized both dental plaque-induced gingival diseases and nonplaque-induced gingival lesions along with seven categories of periodontal diseases and conditions: chronic periodontitis, aggressive periodontitis, periodontitis as a manifestation of systemic disease, necrotizing periodontal diseases, abscesses of the periodontium, periodontitis associated with endodontic lesions, and developmental or acquired deformities and conditions.
Photo Credit: watanyou / iStock / Getty Images Plus

Updating the Classification System
More recently, an organizing committee from the American Academy of Periodontology (AAP) and the European Federation of Periodontology determined that updates were needed to the 1999 classification system. Case definitions, diagnostic criteria, and the addition of peri-implant diseases and conditions were considered as part of the new classification. Findings were discussed at the 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions and presented at the recently held Europerio Conference in June 2018.
Photo Credit: Katerina Sisperova / iStock / Getty Images Plus

Three Main Categories
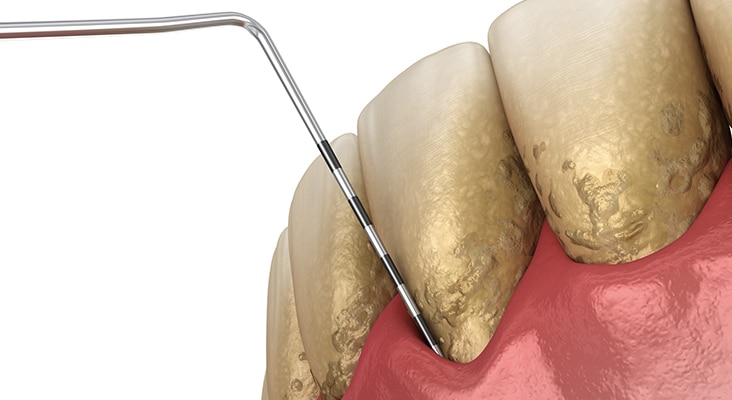
Within this new classification system, periodontal diseases and conditions are divided into three main categories: 1) periodontal health, gingival diseases, and conditions; 2) periodontitis; and 3) other conditions affecting the periodontium. Parameters defined at the 2017 World Workshop specified that bleeding on probing was the primary consideration in setting thresholds for gingivitis. Further, it was noted that a patient with gingivitis can revert to a state of health; however, a patient with periodontitis must be followed for life to prevent recurrence of disease. The classification of periodontitis was modified to recognize three forms of periodontitis: necrotizing periodontitis, periodontitis as a manifestation of systemic disease, and a single category of periodontitis. Staging is established by factors such as clinical attachment loss, bone loss, probing depth, furcation involvement, mobility, and tooth loss. Grading is associated with rate of progression of disease as defined by general health status, smoking, diabetes control, and other individual patient factors that influence disease state.
Photo Credit: agrobacter / E+
Oral-Systemic Link
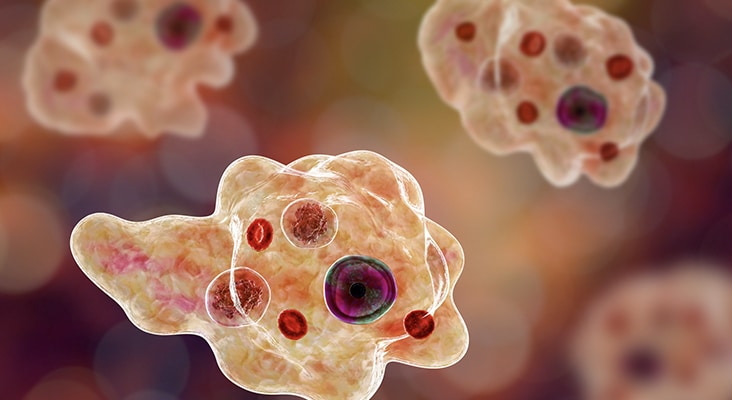
Periodontal manifestations of systemic diseases and developmental and acquired conditions are part of the system. It was recognized that systemic disorders affect periodontal tissues, and these clinical findings should be classified based on the primary systemic disease. Other changes within this category reflect new case definitions combining clinical parameters and evidence.
Photo Credit: TefiM / iStock / Getty Images Plus
Peri-Implant Diseases
The final section of the new classification section relates to peri-implant diseases and conditions. Four main areas were developed: peri-implant health, peri-implant mucositis, peri-implantitis, and peri-implant soft and hard tissue deficiencies. Peri-implant health represents an absence of signs of inflammation and bleeding on probing that exists around implants with normal or reduced bone support. In contrast, peri-implant mucositis consists of bleeding on probing and visual signs of inflammation. This condition can be reversed by eliminating biofilm. Peri-implantitis occurs in tissues surrounding dental implants associated with inflammation in the peri-implant mucosa and progressive bone loss.
Photo Credit: Dr_Microbe / iStock / Getty Images Plus
Opportunity for Dental Hygienists
The new classification system for periodontal and peri-implant diseases/conditions provides an opportunity for oral health professionals to refine their diagnoses and treatment planning procedures. Staff meetings and study club sessions can be held to learn each component of the classification scheme, specific criteria, and case definitions. Discussions can be held to gain consensus on application to practice appreciating that a patient may have multiple diagnoses represented in various sextants or quadrants of the mouth. In addition, practitioners can reflect how to better educate patients so they fully understand their periodontal diagnoses, the extent and severity of disease in each area of their mouth as reflected by staging and grading, and the significance of the proposed treatment plan and anticipated outcomes.

